To ‘D’ or not to ‘D’ – Part 2
Question and Answer Corner
When I wrote the ‘Sunday Read’ on vitamin D back in June 2020, I honestly did not expect the level of positive correspondence back from our readers. Literally, hundreds of you got in contact and I have been truly overwhelmed by the amount of interest it generated.
In addition to the feedback, some of you had further questions on the subject or wanted more details on certain points. In either case, I thought the best idea would be to write a Part 2 in which I would aim to answer some of the more frequently asked questions and address some of the additional points you have raised.
I will be using a ‘Question & Answer’ format with the first name and location of the person who sent the question.
I hope you enjoy reading this article as much as I enjoyed writing it.
Dear Michael,
I am not a patient of your Practice but the rest of my family are. My question is this. I have worked night shift in a factory in Norwich for the last three years. To be honest, I am not a big fan of exercise, I just do not have the stamina or time. I feel I have a good diet with three regular meals. My stumbling block is that I do like a pint or two. I weigh 22 stone, which I know is a problem, but I find it really difficult to lose weight. During the current Covid crisis, I have been told that I am on the NHS ‘at moderate risk’ list, due to my weight. Having read your last vitamin D article, I thought I would ask about the possible problems I could be heading for with respect to vitamin D?
Many thanks, James from Briston
Great question James and one that may resonate with other people. I am going to make an assumption on your height for the purposes of working out your BMI. If you are 6-foot, your BMI comes out at 43. So yes, you do fall within the ‘at moderate risk’ group.
Vitamin D is a fat-soluble hormone which your body makes and stores within the fat cells of your skin. If you carry a lot of excess fat, there is a decrease in the bio-availability of the vitamin D. This is caused by the reduced ratio of vitamin D to fat which leaves most of the vitamin D essentially locked into the body fat compartments.
Furthermore, studies have shown that when grossly overweight individuals are exposed to ultraviolet light, they only raise their blood levels of vitamin D by about 45% compared to a normal weight person. So, roughly speaking, this type of individual needs at least twice as much vitamin D to satisfy the body’s needs, as illustrated in the graph below.
Working night-shifts and needing to sleep during the day, you will probably not get out very much in the sunshine. This, combined with your excess weight, means that you may find it difficult to keep your vitamin D at a healthy level.
There are some other symptoms you should watch out for which may seem unrelated. These include bone pain, muscle pain, lethargy, tiredness and muscle weakness, especially to the lower back, pelvis and hips.
These symptoms can be caused by a condition known as osteomalacia (effectively, the adult version of rickets) which is associated with low levels of vitamin D. Unfortunately, I am seeing more and more of this in people who are in a similar situation to you (health workers, police, security guards, paramedics etc).
Overweight people can experience ‘The Perfect Storm’, i.e., being overweight, having osteomalacia and being vitamin D deficient. It is a vicious cycle, spiralling downwards, out of control.
I had a patient some time ago, who was in a very similar situation to you James and had osteomalacia. His vitamin D levels were assessed as ‘dangerously deficient’, so he went onto a mega-dose of vitamin D for 6 weeks. Together with his GP, we managed to get his employers to put him onto day shifts. In addition, he was strongly encouraged to cycle the 3 miles to work, which in fairness, he took on board and did religiously.
The change in his whole demeanour was astonishing. He could not get enough of the cycling! After 6 weeks, his vitamin D levels had improved into the ‘sufficient’ levels. The mega-dose was cut by 50% and that is where he stayed. Today, his life is a total reverse of what it was, the osteomalacia has gone and with it, all the associated symptoms.
The main thing to establish is: “Find out where you are, before you know where you are going”.
So, my advice James, is to get yourself checked out by your GP and to have a blood test to assess your serum vitamin D levels.
- Best of luck to you. Keep in touch with your progress.
Find out where you are, before you decide where you are going.
Hi Michael
My husband is from India and as such he is classed in the ‘at risk’ group of the population with respect to Covid-19. What is your opinion on this and is there any association with vitamin D as highlighted in some recent newspaper articles?
Vicky from Sheringham
Thank you Vicky. Another fantastic question. Many people presume that someone with darker skin must have adequate levels of vitamin D. To explain why this is not so, we have to go back a few million years…
Vitamin D has been around for some 500 million years, when an ancient lifeform called Phytoplankton roamed the prehistoric seas harnessing the sun’s energy to make vitamin D.
When sea creatures began to venture out of the oceans onto land, they had to overcome the problem of how to obtain adequate vitamin D from their new environment. Vitamin D is vital for adequate calcium absorption. The calcium was needed to create a strong enough skeleton to sustain their body weight on land. So, its effect on life is certainly not a new thing.
Following a further 7 million years of evolution, our ancient ancestors appeared in Africa. Being on the equator, the sun’s position in the sky is pretty much directly overhead. So, the ultraviolet rays are quite intense. Early humans had to adapt to this by increasing the levels of melanin in their skin. Melanin acts like a sunblock. The other characteristic of melanin is raised pigmentation levels in the skin. So, darker skin actually absorbs less vitamin D than fairer skin.
After a further 5-6 million years, they began to migrate out of that continent. Moving away from the equator, the sun’s rays start to hit the earth’s atmosphere at an angle. The further from the equator, the sharper the angle. At certain times of the year the angle is so acute that the ultraviolet light simply bounces off the atmosphere and out into space.
So Vicky, your husband has a double problem. Firstly, the high melanin levels in his skin means he naturally has a high sunblock. Secondly, the UK is so far north of the equator, the ultraviolet radiation is weaker, so it cannot penetrate his skin. This will result in low vitamin D production.
The final consideration is the newspaper articles you mention. The current research into a possible association between vitamin D and immunity has included looking at whether this may be a contributing factor in high mortality rates for Covid in BAME (Black, Asian, minority ethnic) patients. Some very interesting work is being done on this and I will be following it closely over the coming months.
For all the reasons mentioned above Vicky, your husband may wish to begin supplementing vitamin D. There should be no problem with this as long as he has no health risks associated with it (the main one being sarcoidosis). Please contact your GP if in any doubt.
We can’t always get the vitamin D we need from sunshine alone.
Dear Michael
I was fascinated to read about the dangers of over-exposure from the sun versus the application of too much sunblock on my children’s skin, which can lead to a vitamin D deficiency. As a parent, my children’s health is of primary concern, but how am I supposed to get the balance right between too much sun and not enough exposure?
Mary from Docking
There is absolutely no doubt Mary, that too much sun exposure is dangerous. Skin cancer is on the rise and with climate change, the incidence of cases is set to increase. At the Practice, we are seeing more and more cases of erroneous looking moles on people’s skin, even in younger age groups.
But there is no escaping the fact that — without supplementation — 90% of our vitamin D comes from the sun between the months of late April to early September here in the UK. Unfortunately, the ultraviolet radiation we need to work its magic is the UVB type and ‘B’ also stands for ‘burn’ which is exactly what happens when we get too much.
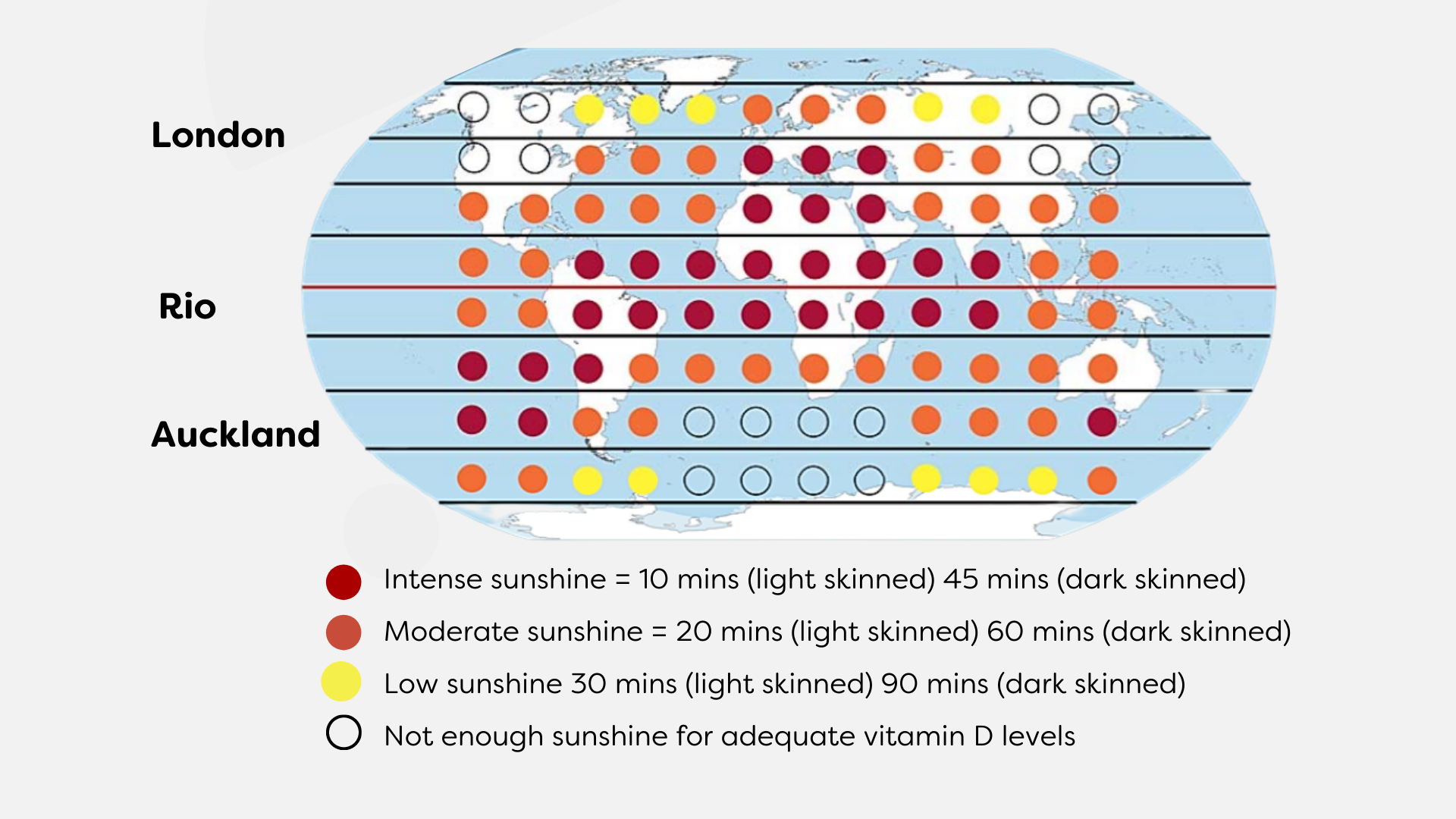
Therefore, it is a fine balance between too much and not enough sunshine. I have included a ‘Sunshine Calculator’ (below) which gives a rough guide to exposure times depending on time of year, location and sun intensity. Always check the daily UV levels though. These are normally given during the TV or online weather forecasts during the Summer. Then adjust timings accordingly.
Another factor to consider is how much time your child spends outside. If they play outside most days, they would need less exposure time per day than a child who tends to spend more days indoors. Always remember, once you feel your child has had enough exposure, slap on the sun protection.
The above information is exactly the same for adults. We all need to take care when out in the sun and take sensible precautions.
Thanks for your question Mary. It always sparks a degree of debate but ultimately, just trust your judgement and use common sense.
SUNSHINE CALCULATOR
Hello Michael
Do you supplement at all and if so, what do you use?
Janet from Wells-Next-The-Sea
Happy to share this with you Janet. Yes, I do supplement a daily dose of vitamin D3, as does my wife. As I have mentioned before, I use the annual altering of the clocks going backwards/forwards to indicate the time to start/stop dosing up for the winter months.
We take a liquid form in which each drop consists of 1000 iu of vitamin D3. I have 5 drops per day with breakfast. The brand is NutriAdvance and each bottle lasts roughly a month. There are several brands available, just ensure you buy from a reputable supplier.
Some people would read this and think negatively about the high dosing levels my wife and I take. But, there are some facts to consider.
When a blood test for vitamin D is carried out, anything under 50 nmol/L will be considered deficient and below 25 nmol/L, severely deficient. As far as general guidelines go, anything above 50nmol/L is sufficient and no further treatment is advised. However, research has clearly shown that, on average, patients with a level of 85 nmol/L will absorb 65% more calcium from a standardised dose of vitamin D than those at 50nmol/L.
At the standard recommended levels, a high proportion of the population would be vitamin D deficient by the end of the winter period. Many will suffer the health-related issues that come with it – persistent pain, mood and behaviour issues as well as fatigue and increased risk of osteoporosis. How many people do you know who suffer from seasonal affected disorder (SAD) in January and February? Interesting!
Thank you for your questions and I hope this has answered some of them. I am really looking forward to tracking the future research on vitamin D and possible links with helping to maintain a healthy immune system, especially in light of the last 12 months and the effects of the Covid-19 pandemic. In the meantime, remain safe and take care.
If you would like to receive Michael’s updates on the latest research and advice on this subject, please fill out the form below.